Theory of Endocrine Immune Surveillance
Posted on October 15th, 2014Pertaining to my clinical veterinary studies, this article was an attempt to share my thoughts with my veterinary profession. The California Veterinarian found my article to be interesting enough to publish it in their journal in January of 1979.
I also created this article titled The Theory of Endocrine Immune Surveillance which I would like to share with you almost 36 years later.
It has taken me all this time to use my theory to help thousands of patients including canines, felines, equines and humans, even though my theory was not accepted then and even now, when it has been proven.
Today’s endocrine immune protocol and treatment plan began with this theory.
For those of you that might be interested in reading more about my clinical research articles, please go to Early Research.
I hope you enjoy the article.
Sincerely,
Dr. AL Plechner
Theory of Endocrine Immune Surveillance
Published in California Veterinarian – January 1979
Alfred J. Plechner, DVM – Los Angeles, California
(Editor’s Note: This theory is presented by Dr. Plechner to stimulate creative thinking and is based upon scientific facts and his own clinical research and observations.)
It is interesting to consider old diseases in modern times. One thinks of those many traditional bacteria, virus, and fungal infections. However, in present times, a clinician is forced to wonder about immunological diseases and ponder the immune system.
Many traditional diseases have been well documented. Detailed studies have carefully delineated the signs of clinical disease that an organism may cause. But in all actuality, does the organism really cause the disease, or does the organism as an antigenic agent elicit a specialized immune response which indeed may cause great damage to the host. Does the staphylococcus bacteria mediate a disease against the body or does the various antigenic compounds in the structure of the bacteria and its various toxins elicit a specific immune response that may destroy adjacent or involved host tissue. Then we are discussing the processing of foreign materials properly with immune conjugation with tolerance of foreign material without inflicting damage to the host while processing these materials. When treating a specific disease with a specific antibiotic, are you then destroying the bacteria which appears to be overwhelming the host response, or are you merely reducing the foreign antigen and removing its antigenicity and reducing the numbers of antigenic bacteria necessary to elicit this specific immune host tissue reaction.
It appears that it is of ultimate importance that the body remains in a state of immune homeostasis, therefore allowing for the proper processing of self antigens and foreign antigens. If this immune homeostasis is altered, then serious self-destructive diseases may occur. The immune system appears to be regulated by the endocrine system and its central point of organization may be mediated through the adrenal axis with central nervous system input through the pituitary, hypothalalmus, and cerebral cortex, etc. Whether agreed to or not, steroids have been as important to clinical veterinary practice as antibiotics. In practice, we all use steroids in various forms for a variety of diseases and generally achieve good results. No one admits to using these substances as frequently as most of us use them, because this is not a popular trend in today’s clinical veterinary medicine. But is this really true? I think not. The experts tell us steroids are usually contraindicated. However, if a practitioner is honest, it becomes quite apparent that steroids are very necessary. Ever since the 1940s when an “X” substance was found at the Mayo Clinic and this research effort sequelled because this substance was “bad”, steroids have often remained in the realm of unacceptable therapy.
With the many uses of steroids and many lifesaving qualities produced by this drug, one wonders if this multipurpose hormone is not one of the most important substances in the body! I believe that cortisol is the mediator of endocrine immune surveillance. I have often wondered if we as practitioners, in giving a patient a steroid, might not merely be replacing in the body a synthetic hormone which acts as a replacement substance, which due to genetic defect or acquired damage does not occur in proper amounts.
A number of years ago, began looking at the adrenal gland for signs of clinical disease. By this time, veterinary pathologists had noted varying degrees of adrenal histopathology often not correlated with clinical disease. With the development and availability of more recent and more direct immunological methods and procedures, I have found good evidence that adrenal disorders exist clinically in veterinary practice and differ from the classic Addisonian and Cushing syndromes.
It is important to understand the anatomy of the adrenal cortex. The adrenal cortex is composed of three basic layers. The most superficial zone is the zona glomerulosa which produces aldosterone, which is necessary for the reabsorption of sodium and the excretion of potassium. The zone is primarily controlled by the reninangiotensin system. This zone is only slightly responsive to ACTH. In man it is suspicioned that ACTH may have a supportive effect on the zona glomerulosa, but chronic ACTH deficiency apparently does not alter the responsiveness of this layer.
The zona fasciculata produces cortisol for glucocorticoid action and I feel is involved clinically, at least in part, in endocrine immune surveillance. This zone is the target area for ACTH and proper cortisol production is necessary to activate the negative feedback mechanisms to the pituitary. The cortisol occurs in two major forms. Cortisol may be bound to albumen, which is biologically active and essential for activation of the anterior pituitary negative feedback system.
Cortisol may be bound to an alpha globulin as transcortin which is biologically inactive for the most part. Interestingly enough, of the total cortisol produced, 5% is in the biologically active state and 95% is in the bound form. Resting blood cortisol levels and ACTH stimulated blood cortisol levels are often measured by radioimmunoassay, which measures total cortisol (free and bound). Theoretically speaking, when resting and stimulated blood cortisol levels occur in proper amounts at the time of testing, are they really normal? The ratio between free and bound cortisol may be abnormal. Adrenal disease may be present therefore, even with normal test levels. With an incorrect ratio between active and bound cortisol, the negative feedback mechanism to the anterior pituitary gland is definitely damaged. It is important to remember that naturally occurring active steroids must have a hydroxyl group at the eleventh position to inhibit ACTH release. It may be necessary to collect 24 hour urine production from a patient to determine the ratio between bound cortisol and biologically active cortisol. The innermost layer of the adrenal cortex is the zona reticularis, which is under the control of ACTH and is responsible for the production of estrogens, androgens, and prostiglandins. In the human being, almost all androgen production in the female occurs in this layer. In the male, two-thirds of the androgen production occurs in the zona reticularis. If this is true in the canine, which I believe it is, then when a complete ovariohysterectomy is performed and a state of urinary incontinence occurs at a later time, there is certainly reason to suspect the zona reticularis is not producing sufficient amounts of the proper hormone. Cystic ovarian disease is certainly suspect and may be primarily or secondarily associated with this layer and may also have an influence or be associated with the zona fasciculata. With production of progesterone from the corpus luteum and concurrent production of estrogenic compounds from the zona reticularis, it becomes a little more apparent why pyometra complex might occur.
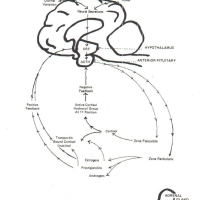
 It is of utmost importance to understand some of the interrelationships of the adrenal cycles. The adrenal stimulation cycle may originate in the adrenal cortex due to diurnal factors or stress producing neural secretions (Figure 1). These and other secretions act upon the hypothalamus to release Corticotropic Releasing Factor (CRF). CRF acts upon the anterior pituitary to cause the release of ACTH. ACTH causes the release of cortisol from the zona fasciculata. If cortisol production is normal, and proper amounts of cortisol occur in the free state, then the negative feedback mechanism functions to stop further ACTH release (Figure 3).
It is of utmost importance to understand some of the interrelationships of the adrenal cycles. The adrenal stimulation cycle may originate in the adrenal cortex due to diurnal factors or stress producing neural secretions (Figure 1). These and other secretions act upon the hypothalamus to release Corticotropic Releasing Factor (CRF). CRF acts upon the anterior pituitary to cause the release of ACTH. ACTH causes the release of cortisol from the zona fasciculata. If cortisol production is normal, and proper amounts of cortisol occur in the free state, then the negative feedback mechanism functions to stop further ACTH release (Figure 3). If, however, the zona fasciculata is malfunctioning and either the ratio of cortisol production between the active or bound state is incorrect, or the actual quantity of cortisol is depressed, then the negative feedback system is damaged and ACTH secretion continues (Figure 4). The ACTH then causes further secretion of estrogens, androgens, and prostiglandins from the zona reticularis.
If, however, the zona fasciculata is malfunctioning and either the ratio of cortisol production between the active or bound state is incorrect, or the actual quantity of cortisol is depressed, then the negative feedback system is damaged and ACTH secretion continues (Figure 4). The ACTH then causes further secretion of estrogens, androgens, and prostiglandins from the zona reticularis.  The significance of this phenomenon is that estrogens and prostiglandins cause biologically active cortisol to go into the bound state as transcortin and therefore cause further damage to the negative feedback system with the anterior pituitary. The estrogen and prostiglandins act then on a positive feedback system to the hypothalamus by causing secretion of CRF.
The significance of this phenomenon is that estrogens and prostiglandins cause biologically active cortisol to go into the bound state as transcortin and therefore cause further damage to the negative feedback system with the anterior pituitary. The estrogen and prostiglandins act then on a positive feedback system to the hypothalamus by causing secretion of CRF.
One can then begin to imagine, if active cortisol is necessary for the proper endocrine feedback schemes to function normally, then certain natural phenomenon may act to cause dysfunction.
If a female canine begins its estrus cycle, and has a genetically induced adrenal disorder, then the estrogens produced during the cycle may shift the active cortisol into transcortin, and then a certain degree of endocrine-immune surveillance is lost. Hypersensitivity diseases may occur due to a hyperactivity of the immune system because cortisol has been bound and is not as available.
A male canine might be stimulated by a female in estrus, and due to increased prostiglandin production, cause a transcortin shift with loss of surveillance and increased immune hypersensitivity. Any disease process, trauma, emotional stress, etc., that damages or fatigues the zona fasciculata can lead to a loss of endocrine-immune surveillance. (Note: Steroids occurring in low levels directly suppress or lyse T-Iymphocytes without effect on the B-lymphocytes, but in higher concentrations may cause suppression of both B and T lymphocytes. In many of the cases we have studied, B and T lymphocytes population are normal, however, the cortisol production is not. Therefore, one can begin to understand how a myriad of environmental conditions can change cortisol levels and concurrently alter the regulation of the populations of B and T lymphocytes. The overall process is certainly much more complex than the above, however, the basics are applicable.)
It is of ultimate importance to realize that estrogens and prostiglandins also cause a shift of certain thyroid compounds to a bound state and thereby may cause a change in the overall metabolic rate. This effect may explain why certain patients are less responsive or non-responsive to classic drug therapy. This may be part of the reason we find one-fourth to one-third of all hypothyroid canines with normal T3 and T4 levels, (Note: In man with subclinical adrenal damage, a state of hyperthermia may exist.) I have noted this same finding with our studies also.
The further one proceeds with this scheme of endocrine immune surveillance, the more it becomes apparent that this is a multisystem scheme of great complexity.
 It appears that cortisol is necessary for catecholamine synthesis in the adrenal medulla, brain, spinal cord, and other nervous tissue (Figure 2). Synthesis of epinephrine at proper levels acts as a negative feedback mechanism involving Corticotrophic Releasing Factor and ACTH. Therefore, if the zona fasciculata is impaired, then cortisol levels are decreased. If catecholamine synthesis is reduced or inhibited then ACTH release is increased due to the damaged negative feedback system from epinephrine and cortisol (Figure 5).
It appears that cortisol is necessary for catecholamine synthesis in the adrenal medulla, brain, spinal cord, and other nervous tissue (Figure 2). Synthesis of epinephrine at proper levels acts as a negative feedback mechanism involving Corticotrophic Releasing Factor and ACTH. Therefore, if the zona fasciculata is impaired, then cortisol levels are decreased. If catecholamine synthesis is reduced or inhibited then ACTH release is increased due to the damaged negative feedback system from epinephrine and cortisol (Figure 5).  Resultant increased estrogen and prostiglandin then further reinforces the cyclic damage. The resultant effect again is the loss of endocrine-immune surveillance. (Note: One might then imagine that with people and animals undergoing great emotional stress, with persistent over-production and synthesis of epinephrine, the cortisol levels would be decreased due to a fatigue of the zona fasciculata with loss of endocrine-immune surveillance, with resultant production of disease.)
Resultant increased estrogen and prostiglandin then further reinforces the cyclic damage. The resultant effect again is the loss of endocrine-immune surveillance. (Note: One might then imagine that with people and animals undergoing great emotional stress, with persistent over-production and synthesis of epinephrine, the cortisol levels would be decreased due to a fatigue of the zona fasciculata with loss of endocrine-immune surveillance, with resultant production of disease.)
I believe that many diseases can be involved primarily or secondarily with adrenal gland disorders. It Is interesting to speculate that the difference between allergy and severe auto-immune diseases and tumors, at least in part, may be the difference of degrees of adrenal malfunction. A tumor, therefore, may merely be an end product due to loss of endocrine-immune surveillance mediated through a multisystem malfunction involving the adrenals, pituitary, thyroid, hypothalamus, cerebral cortex, immune system, and improperly processed foreign and/or self antigens. I further believe that generalized demodecosis, immune complex, or auto-immune diseases, certain endocrine diseases and tumors, have at least in part, one common denominator, which is a damaged adrenal cortex.
Summary
The actual theory of endocrine-immune surveillance indicates that cortisol, produced by the zona fasciculata is the mediator substance for endocrine-immune surveillance. This substance, through its production and modification, acts to regulate, control, and function as the link between the endocrine and immune systems. The other related layers of the adrenal cortex act to further modify the cortisol as a mediator substance and add further centralized regulatory functions for other related systems.
Concerning the theory and the diagrammed cycles, one may further understand that stress can cause increased epinephrine synthesis which may consume and fatigue cortisol production and damage the negative feedback system. The hypothalamic pituitary direct feedback cycles stimulate the zona reticularis which produces and releases estrogens and prostiglandins which further bind active cortisol into bound transcortin which further damages the endocrine-immune surveillance. Certain thyroid compounds are also bound by the estrogen, etc. An overall unresponsive state of immune hyperactivity may then exist with partial to total loss of endocrine-immune surveillance.
Many severe immune mediated diseases appear to be primarily or secondarily involved with the adrenal gland. Generalized demodecosis appears to be involved with an adrenal malfunction. Our own studies have shown a definite genetic transference of generalized demodecosis, at least in part, through a damaged adrenal cortex.
It is of major significance to realize that the degree of damage involving the adrenal cortex may be variable. There are specific disorders involving specific layers of the adrenal cortex. There are definitely a number of diseases that vary from those classic adrenal disorders that we are all familiar with at this time. Normal blood levels may still be produced and measured clinically with severe adrenal damage being present, if enough functional cells remain. Our histopathology and immunopathology studies definitely support this fact. Therefore, normal adrenal test levels do not rule out clinical disease of the gland. The disease may be inherited directly causing early manifestation or may be acquired and develop later in life due to immunological destruction of the adrenal tissue by the host’s own immune system and other diseases.
If cortisol then is the mediator of endocrine-immune surveillance, and varying degrees of adrenal mediated diseases are possible, it is interesting to speculate then that mild adrenal dysfunction might manifest itself as an allergy or hypersensitivity disorder and a more severe adrenal dysfunction might lead to a more serious endocrine immune complex malady resulting in auto-antibody disease and tumors.
Much more research is needed in this area, particularly involving the endocrine regulation and its influence of the endocrine system with its overall effect on the host.